- Influenza A and other respiratory viruses and how to avoid them this winter - January 2, 2026
- Kounis syndrome: the acute coronary syndrome that fuses cardiology and allergies - January 7, 2025
- Physical exercise as a cause of Anaphylaxis - December 9, 2024
Anaphylaxis is an acute, complex, and dramatic event that can be fatal. It results from a rapid, generalized, and severe hypersensitivity reaction mediated by immunological or non-immunological mechanisms. It is characterized by symptoms and signs in the skin, mucous membranes, and organs or systems related to the release of mediators from mast cells and basophils.
The European Academy of Allergology and Clinical Immunology defines it as: “a severe, systemic hypersensitivity reaction that is potentially life-threatening, characterized by rapid onset, respiratory or circulatory problems, and usually, although not always, associated with changes in the skin and mucous membranes.”
The prompt recognition of this episode by the patient, healthcare personnel, as well as institutions (daycare centers, schools, institutes and society in general), and immediate action, can reverse the course of this process.
In the UK, a study showed that hospital admissions for anaphylaxis (from all causes) increased by 61.5% between 1992 and 2012. This underscores the need for societal preparedness to address this situation, which has an estimated prevalence of 0.3% in Europe and 5.1% in the US. However, these data are limited and heterogeneous.
Risk factors for anaphylaxis
There are risk factors that increase the possibility of suffering anaphylaxis and influence the severity of the condition, including age. Advanced age and adolescence are risk factors for fatal reactions, type of allergens, atopic diseases, comorbidities, polymedication, among others.
Bronchial asthma is a relevant risk factor.
Causes of Anaphylaxis
The most frequent ones cause anaphylaxis through IgE-dependent immunological mechanisms, including foods (nuts, fish, shellfish) and additives, drugs such as beta-lactam antibiotics and NSAIDs, insect venom (hymenoptera), aeroallergens, seminal fluid, latex, immunotherapy, among others.
It is important to note that, although immunoglobulin E-dependent immunological mechanisms are the most frequent causes, there is a group of anaphylaxis produced by immunological mechanisms not dependent on IgE, including dextrans, monoclonal antibodies, and others, as well as non-immunological factors such as radiological contrast agents, some NSAIDs, alcohol, cold, heat, solar radiation, and physical exercise, which will be our topic today.
Exercise-induced anaphylaxis syndrome
As we mentioned, physical exercise can cause anaphylaxis or act as a cofactor, lowering the reactivity threshold to an allergen and amplifying the condition.
The most common type is exercise-induced food anaphylaxis. It is clinically characterized by skin reddening, pruritus (itching), urticaria with or without angioedema, and cardiovascular collapse between 2 and 30 minutes after starting exercise.
It is unique in that it can be triggered by eating foods that a person normally tolerates. This could be due to a subclinical food allergy, which manifests itself with exercise and is called “exercise-induced postprandial anaphylaxis.”
The reaction occurs if physical exercise is performed in the 4 hours before or after eating the food in question, frequently cereals, nuts, shellfish or fish.
However, the patient can eat the food to which he is sensitized without suffering anaphylaxis, if he does not exercise during the designated hours; as well as
exercise without suffering anaphylaxis if you do not consume the food within 4 hours before or after eating.
Symptoms
Symptoms develop rapidly and may include:
- Abdominal pain
- Anxiety
- Chest tightness
- Difficulty breathing, laryngeal stridor
- Difficulty swallowing
- Hives, itching, redness of the skin
- Nasal congestion
- Nausea and vomiting
- Palpitations
- Swelling of the face, tongue and eyes
- Loss of consciousness
Treatment
The treatment of exercise-induced anaphylaxis syndrome is fundamentally prophylactic and is based on avoiding the food that, although commonly eaten, is known to be related to anaphylaxis during exercise. Subclinical food allergy has already been mentioned.
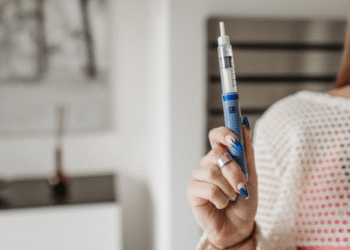
If it appears, physical exercise should be stopped immediately and it should be treated as any other cause of anaphylaxis with adrenaline (drug of choice) 0.5 mg per dose, IM in adults and in children 0.01 mg/kg per dose IM maximum 0.5 mg, being able to repeat the dose every 5-10 min if necessary.
If there is glottic edema, administer nebulized adrenaline 1-2 ml after IM adrenaline. Administer oxygen therapy, assess whether orotracheal intubation is necessary. Fluid therapy for hemodynamic stabilization with physiological serum (PS) 10 ml Kg in the first 10 minutes, 1-2 liters in the first hour, with the aim of normalizing blood pressure (BP). In patients with cardiovascular or renal disease, monitor for fluid overload. Children are administered PS at 20 ml/kg every 10 minutes until BP stabilizes.
Other second-line medications are used to alleviate symptoms: antihistamines, corticosteroids, antiemetics, bronchodilators, among others. For adult patients who are on beta-blocker therapy and respond poorly to treatment with adrenaline, administer Glucagon 1-2 mg intravenously as a bolus followed by an infusion of 0.05-0.1 mg/kg/hour. In children, 20-30 mcg/kg as a bolus followed by an infusion of 5-15 mcg/min.
In our medical practice we have seen patients with this clinical picture in whom it is sometimes difficult to demonstrate the cause-effect relationship, so after the initial treatment aimed at stabilizing the patient's condition, the patient should be referred to an allergist for study.
“Knowing what to do reduces fear”
Rosa Montero