- What is rosacea and how to recognize it? - February 3, 2026
- Impetigo: what it is and when to seek medical advice - February 2, 2026
- Bactrim in Spain: what is its equivalent in pharmacies? - February 1, 2026
Many women with polycystic ovary syndrome (PCOS) do everything right and still don't lose weight. This is frustrating and has a medical explanation. The medical approach to weight loss with PCOS usually begins with lifestyle changes, and if there is a metabolic risk, metformin may be considered as supportive treatment.
In many patients, the focus is on improving insulin sensitivity and the cardiometabolic profile. The goal is not just to "eat less." It's to make the body respond better.
When you meet with an endocrinologist, the focus is often on two things. Understanding why your body is resisting weight loss.And finding realistic ways to move the needle while keeping your health safe.
Beyond diet: the hormonal approach
PCOS isn't just an ovarian problem. In many patients, the core issue is metabolic. Insulin resistance can cause the body to produce more insulin to manage glucose. This can lead to fat storage in some people. It can also affect appetite and energy levels.
That's why endocrinologists often look beyond the scale. They ask about menstrual cycles, acne, body hair, hair loss, and family history. They also ask about sleep, stress, and eating patterns. These are clinical data, not just "details.".
During a consultation, it's common to order a lipid profile and glucose tests, ideally an oral glucose tolerance test (OGTT), and routine insulin prescriptions are not recommended. With this information, the doctor estimates your metabolic risk and defines priorities. Sometimes they also check thyroid function or other parameters if there is clinical suspicion. The goal is to rule out additional factors and personalize the treatment plan.
At this point, it's important to clarify something. There isn't a single diet for PCOS, but some women find it helpful to choose low-glycemic-index carbohydrates to smooth out blood sugar spikes. This is one possible strategy, but not the only valid one. What usually matters most is that the plan is sustainable and appropriate for your individual situation.
Exercise is also part of the treatment. The goal is to improve insulin sensitivity and body composition. In addition to cardio, strength training is often especially helpful within the exercise plan. It helps maintain or build muscle, which improves how the body uses glucose throughout the day.
Metformin: Does it help with weight loss for PCOS?
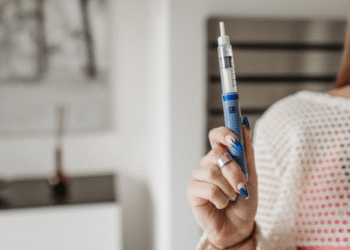
Metformin is frequently used in PCOS for metabolic purposes, although its official indication in Spain is type 2 diabetes. It is not a "weight-loss" drug. In selected patients, it can help improve insulin resistance. In some women, this change facilitates some weight loss; in others, the effect on weight is modest.
The important thing is to understand what it can and cannot do. Metformin is not a substitute for a healthy diet and exercise plan. It usually works as a supportive treatment when there is metabolic risk, prediabetes, or other associated conditions. The decision depends on your medical history and test results.
If prescribed by a doctor, digestive tolerance is also assessed. Some people experience nausea or diarrhea initially, which is why monitoring is important. Contraindications and safety are also reviewed in each case.
Metformin is contraindicated in cases of reduced kidney function, for example with a GFR below 30, and it is not routinely recommended during pregnancy and should be individualized with your doctor.
If you're also exploring medications that are associated with weight changes, it's important to put them into context. For example, bupropion (Wellbutrin) can affect weight in some people, but it's used for specific indications.
The importance of a multidisciplinary approach
In practice, the most effective approach to PCOS is usually a team effort. The endocrinologist handles the metabolic aspects. The gynecologist assesses the reproductive and hormonal components. The family doctor coordinates and monitors the treatment, and a registered dietitian nutritionist can translate the theory into a realistic and sustainable routine.
In the public healthcare system, you'll usually start with your primary care physician. They'll typically order initial tests and refer you if necessary. In the private system, you can see an endocrinologist sooner, but in both cases, it helps to have a clear summary: symptoms, medication, and any previous lab results you may have.
Realistic goals are also discussed. Sometimes, losing a moderate percentage of weight improves metabolic cycles and markers. An extreme transformation isn't always necessary. What is necessary is a plan that doesn't break you inside, either physically or mentally.
This content is for informational purposes only and does not replace medical advice. Review the official package insert for the medication and follow the instructions of your doctor or pharmacist before starting or changing any treatment.